 About Babies Born Small
About Babies Born Small
Here is an explanation about babies born small, typical diseases found in babies, development, nutrition, and raising twins and triplets.
Babies
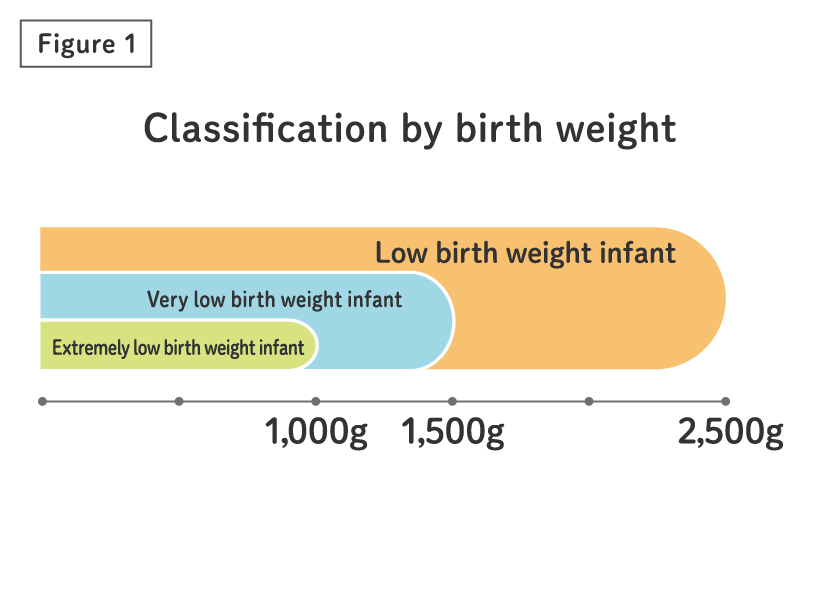
Babies can be grouped according to their birth weight and gestational age (how long the baby was in the mother's womb) as follows. The terms low birth weight infant, very low birth weight infant, and extremely low birth weight infant are used for babies that weigh less than 2,500 g, 1,500 g, and 1,000 g respectively. Extremely low birth weight babies and very low birth weight babies weigh less than 2,500 g so they are included as low birth weight babies (Figure 1).
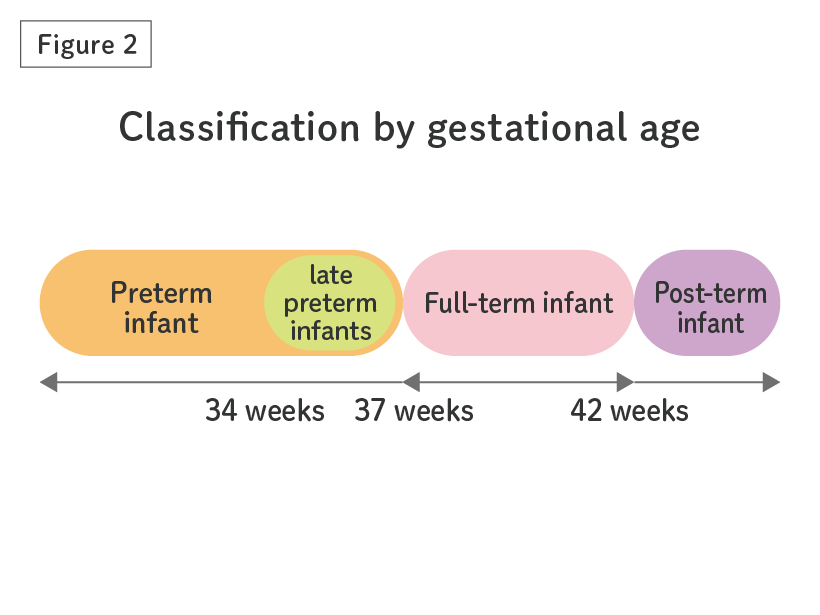
When classified by gestational age, babies born between 37 to 42 weeks (37 weeks 0 days to 41 weeks 6 days) may be referred to as full-term infants, and those born before 37 weeks (36 weeks 6 days) as preterm infants. If the baby is born at or after 42 weeks the term post-term infant may be used (Figure 2).
Today, about 9% of babies are born with low birth weight and about 6% are born preterm.
Babies who need extra support, regardless of birth weight or gestational age, will spend time in the NICU.
About babies born late preterm
Preterm infants born between 34 weeks and 36 weeks and six days of gestation (late preterm infants) usually have a large body build and are delivered in obstetric clinics. Therefore, it is often thought that their care, which is seemingly similar to that for full-term infants, would be fine. However, their whole body is actually immature, they have difficulty breastfeeding, and are more likely to develop diseases, such as respiratory problems, jaundice (a condition in which the skin turns yellow as a result of accumulation of excess bilirubin), hypoglycemia, and low body temperature, than full-term infants. It has been reported that they are at risk of incomplete nervous system development over the long term if appropriate treatment is not provided. Even if they are born without any apparent problems, they require careful observation for the development of the symptoms described above.
Typical Diseases
Babies born small may be at some risk because they are "missing something" or "premature." The NICU and GCU will help these babies adapt. Here is an explanation on typical symptoms and diseases that can be seen in babies born with a gestational age of less than 34 weeks. What is introduced here does not happen to all babies, but it is not uncommon if such symptoms or disease are found, and the doctors and nurses who work in the NICU understand them to give the appropriate treatment and care.
Respiratory System
There are many tiny air sacs in the lungs called alveoli that carry oxygen and carbon dioxide in and out. Pulmonary surfactant, a substance like liquid soap, is secreted into the alveoli to prevent the alveoli from collapsing when you exhale. The lungs of babies born before 37 weeks of gestation are underdeveloped and it may be difficult for the alveoli to expand due to insufficient secretion of this pulmonary surfactant.
To prevent this, steroids may be injected to pregnant mothers who are expecting to give premature delivery. Treatment after the delivery involves injecting the artificial surfactant into a tube inserted into the trachea (surfactant replacement therapy). This tube may be removed immediately if breathing improves, but some babies may require a ventilator for days or weeks.
Babies born premature and small, may have lung damage due to infections from amniotic fluid and/or the use of postnatal ventilators. This can lead to long-term deterioration of lung function, requiring oxygenation and/or mechanical ventilation. This is diagnosed at 28 days after birth or at 36 weeks of the corrected age week (weeks based on the due date), whether oxygen is required and with or without respiratory support. In severe cases, it may cause complications such as "pulmonary hypertension" and may affect his/her respiratory function in later childhood.
As a treatment, we consider shortening the period of using the ventilator or using ventilation that is gentle to the lungs as much as possible. In addition, treatment such as adjusting the oxygen administration concentration, adding artificial surfactant, administering steroids, or water restriction / diuretics (drug that helps produce urine) are administered.
Because the baby's ability to control breathing (respiratory center) is immature, the rhythm of breathing may become faster or slower. Especially, babies born early sometimes hold their breath for a period of time, which can lead to low oxygen levels or low heart rate. The symptom can be divided to "obstructive" where the airways are blocked, or "central" in which signals from the brain cannot be sent, but in most cases it is a mixture of both.
For treatment of the "obstructive" types, air or oxygen is delivered to widen the airway and support breathing, and for the "central" types drugs such as caffeine is used to promote breathing. In fact, both of these treatments are used while waiting for the baby to mature.
In utero, fetal lungs are filled with lung fluid and develop with it while maintaining a certain capacity. Lung fluid plays an important role for fetal lung development. However, when babies are born, they start to breathe with their lungs. For that reason, lung fluid must be rapidly absorbed into the lung capillaries and lymphatics soon after birth. The mechanism for this absorption process is astonishing. During late gestation, the fetus in utero begins to prepare for this absorption process in preparation for birth. However, if problems that prevent the lung fluid from being absorbed occur (premature birth, stress before and/or after birth, neonatal asphyxia, etc.), excessive fluid will remain in the lungs, causing respiratory problems. This disorder may occur to babies even in full term gestation.
As the name suggests, the symptom of this disease is transient and mostly improves with administration of oxygen or use of a nasal mask. Some cases might require mechanical ventilation, and we need to pay careful attention to them for a while after birth.
Respiratory syncytial virus (RSV) is one of the viruses responsible for the common cold in childhood. It is said that almost all children will have an RSV infection by the age of two. Common symptoms include fever, runny nose, and coughing. If the infection reaches the bronchi, small bronchi, or lungs, infants may develop bronchitis, bronchiolitis, or pneumonia. If infants cannot take meals or drink milk due to respiratory distress as shown above, they may need to be admitted to hospital. For infants with extreme prematurity, lung diseases, heart conditions, immune deficiencies (immune deficiency is a condition in which body's immune system is not fully functioning, which results in a reduced ability to defend against infections) and/or 21-trisomy (infants with Down syndrome), an RSV infection can easily become severe. If your baby develops symptoms such as fever, runny nose, coughing, or other symptoms, you need to pay close attention. Because there is no specific drug for RSV itself, medical treatment such as medication to reduce symptoms, inhalation therapy (treatment using inhaled medication), oxygen administration, mechanical ventilation support can be used to relieve developed symptoms rather than to eliminate the causes of diseases. So, it is important to identify how to prevent respiratory syncytial virus infection.
Meconium Aspiration Syndrome (MAS) occurs when a newborn inhales a mixture of meconium (the baby's first stool) and amniotic fluid during or shortly before delivery. This can lead to airway blockage, respiratory distress, and inflammation, potentially causing pneumonia. MAS is more common in full-term infants, especially if the baby experiences physiological stress before or during birth, which may trigger the passage of meconium into the amniotic fluid, or if there is oxygen deprivation (hypoxia) before delivery.
In some cases, MAS can also affect the baby’s circulation (blood flow) and central nervous system (brain and spinal cord), leading to more severe complications. Intensive care is often required, including mechanical ventilation, intravenous fluids, and medication to manage sedation and other needs. While the overall prognosis for MAS is not necessarily poor, the severity of the condition depends on the extent of oxygen deprivation and multi-organ failure caused by impaired blood circulation.
Cardiovascular System
Before babies are born, they are in the amniotic fluid and does not breathe using their lungs. Therefore, before they are born, most of the arterial blood (blood that absorbed plenty of oxygen) delivered to the lungs will not be sent to the lungs, but delivered throughout the body from a bypass called the "ductus arteriosus" that connects the pulmonary arteries and the aorta (see figure). After birth, the ductus arteriosus is no longer necessary and will close completely because the baby will start breathing from the lungs. However, for babies born premature and small, this ductus arteriosus may be hard to close, and the blood pumped to the aorta will flow back into the pulmonary artery. When this happens, much of the blood will flow into the heart, while organs such as the brain and kidneys will run out of blood.
For treatment, the goal would be to close the ductus arteriosus. One procedure would be to limit fluid in order to reduce the amount of blood flowing through the ductus arteriosus, thus reducing the strain on the heart. The second procedure would be to use drugs such as indomethacin and ibuprofen to prevent the ductus arteriosus from expanding. If these procedures do not work, or if these drugs aren't available, surgical procedures will be taken to closes the ductus arteriosus.
【Trivia】
Indomethacin and ibuprofen may sound familiar. These are used as antipyretic analgesics in adults.
"Late-onset Circulatory Collapse" is a condition that can be seen in babies born prematurely and small around the second week after birth. Babies born prematurely have immature organs, and it is known that the Late-onset Circulatory Collapse is caused by a deficiency of a hormone called cortisol secreted from an organ known as the adrenal gland. This leads to an immediate drop in blood pressure and less urine.
Various treatments can be used for these symptoms, but most of the time steroids are used to supplement the effect of cortisol.
Some neonates admitted to the NICU are diagnosed with congenital heart disease (CHD), a condition characterized by abnormalities in the structure or function of the heart that are present at birth. There are many types of CHD, each requiring careful evaluation and management. Collaboration between pediatric cardiologists and neonatal specialists is crucial for accurate diagnosis and effective treatment.
Digestive System
Normally, meconium contained in the intestines of the fetus is gradually passed after birth. However, premature babies born small cannot pass the meconium well and their intestines become clogged. Depending on the facility, this may also be called "meconium disease" or "meconium ileus". If the stool does not pass you may think it is only constipation, but in the case of a baby born small, air flows into the intestines and the stomach becomes bloated and painful. If this gets worse, the intestines may tear and emergency surgery will be required so this needs to be observed with care.
For this reason, babies who are at risk of this disease will use enema for the stool to pass, but if this is not effective a contrast medium may be injected through the anus or stomach to soften the meconium.
Babies born prematurely and small have an immature intestinal function which may decrease the blood flow to the intestine or disturb the intestinal environment. This can cause inflammation in the intestines and the intestinal tissue may become necrotic. If vomiting or abdominal tension is observed, the cause may be necrotizing enterocolitis and blood test and X-ray will be used for the diagnosis.
For treatment, the condition may improve by simply deflating the stomach and giving antibiotics in a fasted state, or emergency surgery may be required. It is said that giving breast milk first and administering good bacteria such as bifidobacteria are effective in preventing necrotizing enterocolitis.
Brain / Nervous System
In the NICU, you may be told that "the first three days are very important". This is because intraventricular hemorrhage is most likely to occur at this time. Babies born small have fragile blood vessels in the area called the germinal matrix layer of the brain which have a risk of bleeding easily (see figure). This will be diagnosed using ultrasonography (echo), and the degree of bleeding can range from limited bleeding inside the ventricles to widespread severe bleeding. If this is severe, the risk of having an aftereffect will be higher.
If the bleeding is mild this will be followed by observation, but after the bleeding, a condition called hydrocephalus in which cerebrospinal fluid (the fluid that flows between the membrane surrounding the brain and spinal cord) may accumulate in the ventricles and give pressure on the brain. In this case, a surgery may be performed to improve the flow or remove the fluid.
Blood vessels which deliver blood to the brain include those that lead from the surface of the brain to a part called the " Cerebral ventricle" that is deep in the brain, and those that lead from the ventricle to the surface of the brain. Since the blood vessels of these babies born small are underdeveloped, the area called "white matter" where there is little blood flow from these blood vessels will not have enough blood, and the cells here will be damaged (see figure). Severe damage in this area will cause aftereffects such as paralysis. Periventricular leukomalacia can be grouped to diffuse (spreading) PVL and cystic (bag-shaped) PVL depending on how the damage was done. Severe cases can be found using an ultrasonography, but in some cases they are found by taking an MRI before discharge. If the baby is born with a gestational age of less than 28 weeks or less than 1,500 g, this is often checked by taking the MRI of the head before discharge.
Unfortunately, there is no radical treatment yet, but PVL is found when leaving the hospital, interventions such as rehabilitation can be provided at an early stage, so there are advantages to undergo the examination.
The blood vessels of the retina at the back of the eyes of a baby born prematurely and small are underdeveloped and growing rapidly. When a baby is exposed to various stresses and oxygen during this growth, the blood vessels in the retina will grow abnormally, which can lead to poor vision and blindness.
For babies with a short gestational age, eye examinations begin about two weeks after birth. If any abnormalities are observed at this time, areas of the retina where blood vessels have not yet grown may be treated by laser. Depending on the facility, drugs that suppress the overgrowth of blood vessels may be injected into the eye.
【Trivia】
When having an eye checkup, it is very stressful for the baby to have eye drops used and having their eyes opened. Therefore, the examination is carried out once every 1 to 2 weeks. Please praise your baby after the examination.
Blood / Nutrition
Jaundice is a condition in which the skin turns yellow due to the accumulation of a substance called bilirubin in the body. Jaundice is common in newborns, even if they are not prematurely born small. The baby inside the womb receives oxygen from the mother, but the oxygen concentration is low compared to when oxygen is taken in from the atmosphere, so they have different types of red blood cells. When they are born this is replaced with normal red blood cells, and bilirubin is produced in this process. Babies cannot process these bilirubin efficiently, thus the symptoms of jaundice can be seen more often. For babies born prematurely and small, there is a possibility that bilirubin attaches to the brain tissue, which is called "bilirubin encephalopathy (kernicterus)". Bilirubin encephalopathy may have aftereffects such as cerebral palsy.
Jaundice can be prevented using phototherapy. Bilirubin can be changed to a form which can be easily discharged by shining a special light to treat jaundice. If the phototherapy does not improve the symptom and there is a risk of bilirubin encephalopathy, a method called "exchange transfusion" may be taken.
【Trivia】
Phototherapy is a prophylactic treatment to prevent the risk of bilirubin encephalopathy. Therefore, even if the baby is exposed to the light, it does not mean that your baby is at high risk of cerebral palsy.
Babies born prematurely and small can become anemic for a variety of reasons. Some of the main causes can be insufficient supply of iron which should have been supplied while in the womb, functions to make the red blood cells is immature, red blood cells are being replaced (see description of Jaundice), or loss of blood for sampling.
The shorter the gestational age, the more severe it may become and blood transfusion may be required. For other treatments, hormones that make red blood cells will be replenished or iron supplements may be given orally.
【Trivia】
Iron supplements are also one of the prescriptions that babies born prematurely and small receive when they are discharged from the hospital. Some babies do not like this supplement, so please receive tips from the staffs at the NICU and GCU on how and when to give this.
The important components that make up your baby's bones are “calcium'' and “phosphorus.'' In the uterus, calcium and phosphorus are actively transported to the fetuses via the placenta, and their bones are growing rapidly towards the end of pregnancy. However, premature infants cannot always get an adequate supply of calcium and phosphorus. Breast milk alone does not have enough nutritional elements for appropriate bone growth after birth. Moreover, the supply of those elements after birth is less efficient than that in the uterus. As a result, preterm infants are more likely to develop osteopenia.
To prevent this, we can administer calcium and phosphorus preparations in a well-balanced manner through an intravenous drip immediately after birth. Adding fortified breast milk powder, which is high in calcium and phosphorus, can make up for the deficiency.
Development
Corrected age for babies born small
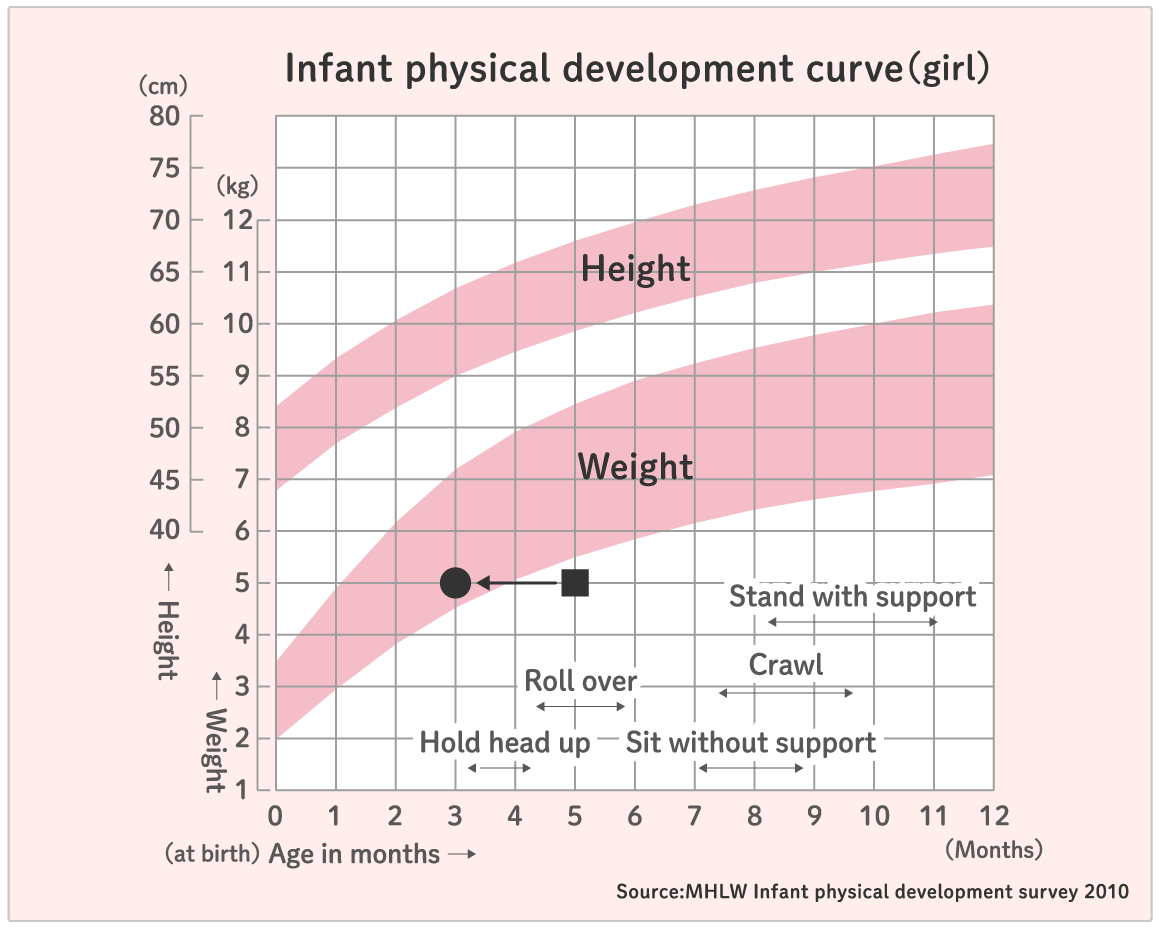
When babies are born prematurely and small, many mothers often worry if the baby is growing up on schedule. Looking at the height and weight graphs in the Mother and Child Handbook, mothers may be worried that the baby is smaller than average or has not yet learned to roll over on his/her own. The baby, born before the expected date is small and immature so it is natural that the baby has a smaller physique and slower development compared to the average if you calculate from his/her birthday. In this case, the corrected age based on the expected date (assuming that the baby was born on the expected date) will be used.
For example, when a girl born two months earlier than the expected date is five months old (the calendar age counted from her birthday is five months), and she weighs 5 kg and can hold her head up but cannot roll over, a mother may be worried when looking at the graph (see ■ mark in the graph). However, the corrected age will be 2 months earlier, at 3 months (see ● mark in graph). Therefore, the fact that the baby cannot roll over is not a problem.
Automatic calculation of the corrected age
Select the expected date of delivery from the calendar and click the Calculate button.
Expected date of birth
Corrected age
{{ result_age }}year(s){{ result_month }}month(s)
Nutrition
Breast milk is the best nutrition for babies but for babies born small, it is even more important. Breast milk contains components that act on immunity, protect against inflammation and excess oxygen, promote growth, and also contains hormones. Breastfeeding promotes intestinal development in preterm infants, prevents enteritis, infectious diseases, and gastrointestinal allergies, as well as reducing the risk of readmission, and improving cognitive (visual) ability. It may be difficult to breastfeed directly at first, so if the mother is in a good health condition, it is a good time to start expressing milk. At first the baby is small so he/she will only need a small amount, but express as much milk as you can to support his/her growth and aim to continue breastfeeding and milking for a long time.
Milk (artificial milk) or breast Donor milk (donated breast milk) may be used if the doctor or obstetric nurse determines that it is necessary considering the health of the baby or mother. A mother does not have to worry that it's not purely their own milk, but to know that it is important to get the required nutrition in a way that suits the baby. Breastfeeding may not work as expected, but it is important to do it in a way that adapts to the mother's physical condition. If you have any difficulties, please consult with a medical staff such as a nurse.

How to pump breast milk
A very small amount of milk should ooze out of your breasts immediately after giving birth. Depending on your health condition, start massaging your nipples and breasts as early as possible. Expressing breast milk every three to four hours promotes hormones to be secreted inside your body, and the amount of breast milk your body creates will increase gradually. Hand milking is good, however, suctioning and stimulating expression of breast milk using a breast pump increases secretion of hormones and will ease your burden. If long-term expression of breast milk is required, the use of a breast pump is recommended.
The amount of breast milk you can produce depends on your food and fluid intake, level of physical and mental fatigue, and other factors. Many mothers become anxious if the amount of breast milk they produce does not increase. First of all, try to make it a goal to maintain the secretion volume. Get advice from nurses and/or midwives rather than worrying about it alone.
Click here for detailed information on expression of milk.
※Linked to external website.

Twins and Triplets
Today, about 1 in 50 babies born are twins or triplets (multiple birth babies). Multiple birth babies are often born small, but in their first year of life they show a remarkable increase in both their height and weight. Motor and language development may be slow but will progress. Children are independent with a personality of their own and it is important not to compare their development.
When multiple birth babies are born, there will be more happiness and fun memories at home but you will require much manpower to take care. Please check the available public services and discuss with the family about the daily support after the baby is discharged. Joining the Multiple baby childcare club and receiving advice may help the daily childcare as well.
Please do not try too hard thinking "because I am a mother".

Linked to external website
Are you sure you want to continue?
* you may not be able to access this website depending on your environment. Please be aware.
